Optimizing MSCs Transplantation for Treatment of Ischemic Stroke Using a Nanofiber Hydrogel Scaffold

Optimizing MSCs Transplantation for Treatment of Ischemic Stroke Using a Nanofiber Hydrogel Scaffold
Adario Chirgwin-Dasgupta (1), Bao Linh Pham (2), Samir Gouin (3), Yin Nan Huang (2)
(1) Medicine, Faculty of Medicine, McGill University, Montreal, Canada
(2) Medicine, Faculty of Medicine, Université de Montreal, Montreal, Canada
(3) Neuroscience, Faculty of Science, McGill University, Montreal, Canada
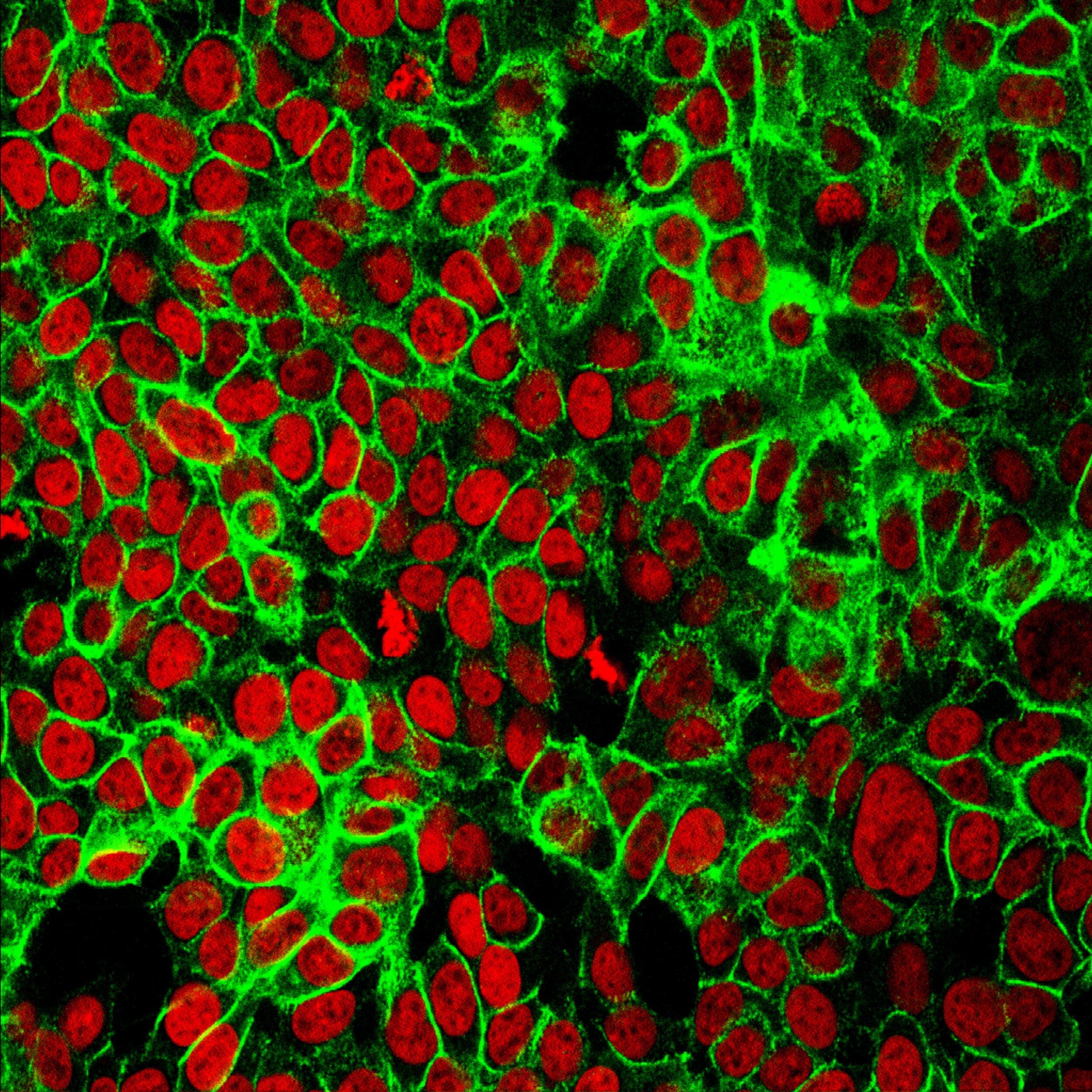
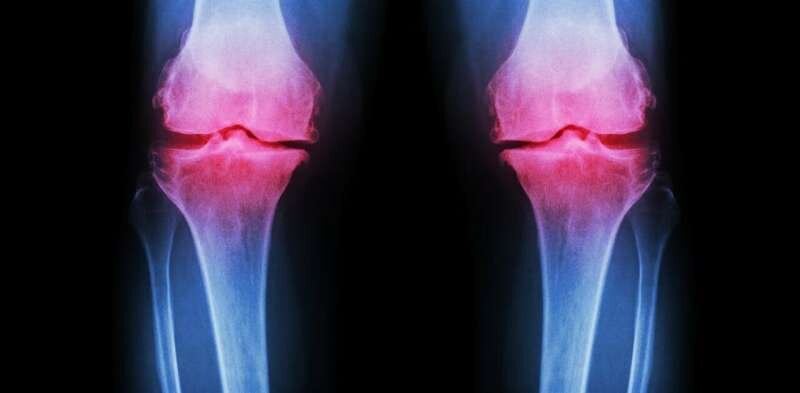
Stroke occurs in more than 60,000 Canadians every year and is the primary cause of physical disability [1]. Current treatment strategies, such as reperfusion and neuroprotective agents, are only available to a minority of patients and have limited benefits [2]. Recent clinical trials have identified stem cell therapy as a promising approach to promote neurorecovery. However, administration methods and molecular factors must be optimized in order to improve graft implantation, cell survival, and new synapse formation. Nanofiber-hydrogel scaffolds (NHS) have shown to improve cell survival and neurite alignment, possibly favoring synapse formation, but have yet to be tested in living stroke models [3]. Our aim is to determine whether delivery of stem cells seeded onto a NHS can optimize graft implantation and synapse formation. GCaMP transgenic mice with induced middle cerebral artery occlusion will be used to assess the implantation of NHS seeded with iPSC-derived MSCs. Experimental groups will receive either MSCs alone or MSCs-NHS. MSC localization and functional integration will be evaluated with calcium imaging and motor function will be assessed using the neurological severity score at specific time points. Synapse formation will be assessed using SV2A PET in vivo [4,5] and immunofluorescence ex vivo. MRI will quantify glial scarring and tumor formation at these time points. We expect significantly greater improvement of all parameters in the MSCs-NHS group, particularly, a correlation of fewer adverse effects with high localization accuracy. The development of an effective neuroregenerative therapy would be a major advance in the management of stroke patients who cannot undergo reperfusion therapy.
Key words: stroke, stem cell therapy, nanofiber-hydrogel scaffold, induced pluripotent stem cells
Références
1. Heart and Stroke Foundation. (Dis)connected: How unseen links are putting us at risk, 2019 Report on Heart, Stroke and Vascular Cognitive Impairment
2. Benedek A, Cernica D, Mester A, et al. Modern Concepts in Regenerative Therapy for Ischemic Stroke: From Stem Cells for Promoting Angiogenesis to 3D-Bioprinted Scaffolds Customized via Carotid Shear Stress Analysis. Int J Mol Sci. 2019;20(10):2574. Published 2019 May 25. doi:10.3390/ijms20102574
3. McMurtrey RJ. Novel advancements in three-dimensional neural tissue engineering and regenerative medicine. Neural Regen Res. 2015;10(3):352-354. doi:10.4103/1673-5374.153674
4. Lyu X, Toyonaga T, Deng G et al. Monitoring synaptic loss in a rat model of stroke: a PET imaging study with [18F]SynVesT-2, radiotracer for the synaptic vesicle protein 2A (SV2A). J Nucl Med. 2020;84(61)
5. Cai Z, Li S, Matuskey D et al. PET Imaging of Synaptic Density: A New Tool for Investigation of Neuropsychiatric Diseases. Neurosci Lett. 2019;691:44-50. doi:10.1016/j.neulet.2018.07.038
Image de couverture : https://commons.wikimedia.org/wiki/File:Bluthirnschranke_nach_Infarkt_nativ_und_KM.png